Anticancer chemotherapy in teenagers and young adults: managing long term side effects
BMJ 2016; 354 doi: https://doi.org/10.1136/bmj.i4567 (Published 07 September 2016) Cite this as: BMJ 2016;354:i4567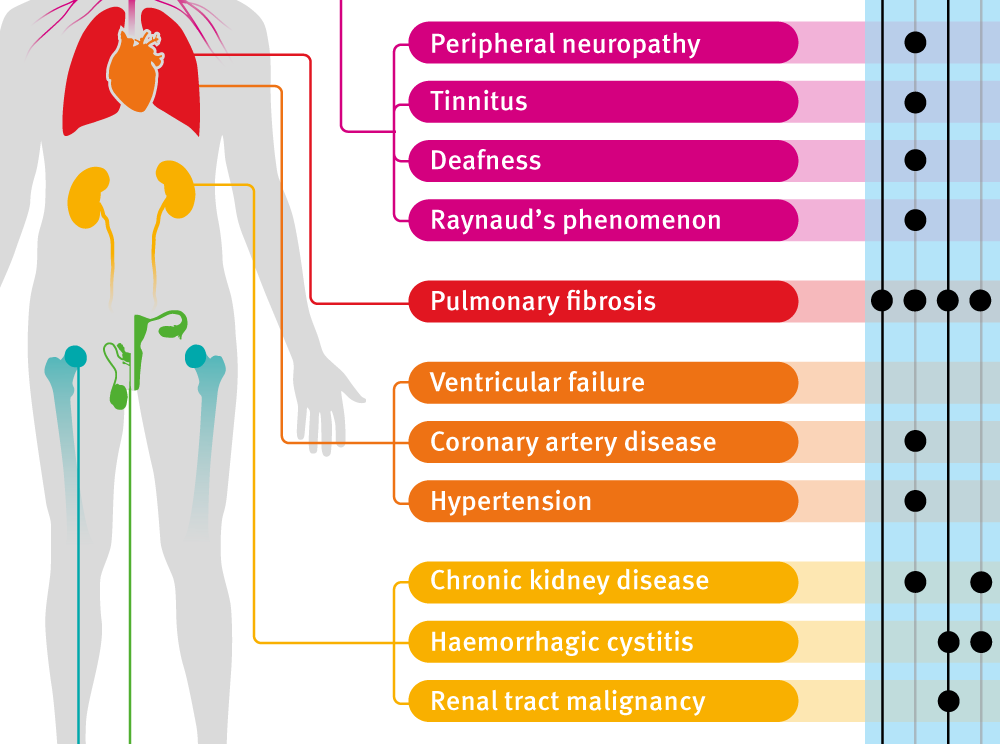
Infographic available
Click here for a visual overview of long term side effects, including principal causitive drugs, risk factors and management of those at risk.

Chinese translation
该文章的中文翻译
- Saif S Ahmad, academic specialist registrar in clinical oncology1 2,
- Marika AV Reinius, core medical trainee1,
- Helen M Hatcher, consultant medical oncologist1,
- Thankamma V Ajithkumar, consultant clinical oncologist1
- 1Department of Oncology, Addenbrooke’s Hospital, Cambridge University Hospitals NHS Foundation Trust
- 2MRC Cancer Unit, University of Cambridge, Cambridge Biomedical Campus
- Correspondence to: S S Ahmad saif.ahmad{at}nhs.net
What you need to know
Side effects of anticancer chemotherapy in teenagers and young adults (TYAs) may occur decades after initial treatment
Ensure patients and care providers have access to details of the treatment received and the potential side effects that may occur
Have a low threshold for suspicion of second cancers and discuss participation in routine cancer screening programmes
Actively ask about psychosocial issues in TYAs at follow-up
Offer referral to fertility preservation services to all TYAs before cytotoxic chemotherapy
Cancer is the leading cause of disease related death in teenagers and young adults (TYAs) in Western countries.1 2 In the UK, cancer in TYAs accounts for 9% and 15% of all male and female deaths respectively, and its incidence has risen by 19% since the mid-1990s, leading to 2300 new cases a year between 2011 and 2013.1 In Japan it accounted for nearly 7000 deaths between 2000 and 2006.3 TYA cancer survivors are likely to live for many decades but are at risk of late effects of their treatment. This article provides information for generalists on late effects of anticancer chemotherapy (see infographic and supplementary table A) that may affect quality of life. Radiotherapy related effects are not discussed but are summarised elsewhere.4
Defining teenagers and young adults
There is no internationally accepted age definition for TYAs. In the UK, TYA age is 15-24 years, whereas the US National Cancer Institute defines adolescents and young adults as aged 15-39 years. In this review we use the UK definition of 15-24 years.
Sources and selection criteria
This article is an evidence based review of late effects of chemotherapy in teenagers and young adults (TYAs). Our review encompasses studies using all age ranges termed as TYA or adolescents and young adult (AYA). We searched PubMed and the Cochrane databases between 1990 and 2016 using the search terms “teenage and young adult cancer, adolescent and young adult cancer, TYA, AYA, late effects, chemotherapy, survivorship” to identify observational studies, randomised trials, meta-analyses, and systematic reviews.
Types and prognoses of cancer in TYAs
Table 1⇓ lists the most common cancers seen in TYAs. The most common cancers seen in this age group are lymphomas, carcinomas (such as breast, bowel, cervix, and thyroid), and germ cell tumours. Survival rates for these TYA cancers are generally good, with five year survival around 85%.5 Five year survival for Hodgkin’s lymphoma and germ cell tumours is more than 90%, but sarcomas such as osteosarcoma (60% survival) carry worse prognoses.6
Top eight cancer types by age group (data from Cancer Research UK)
Chemotherapy plays a major role in the treatment of these cancers, and TYAs are potentially exposed to a wide range of chemotherapy agents, each with distinct late effects. A comprehensive literature review highlighted that these effects are generally different from those seen in younger children and adults, specifically in terms of cardiac toxicity, second malignancies, pulmonary complications, and psychosocial difficulties.7 The reasons for this are not fully established, but it is partly because younger patients receive more intensive chemotherapy regimens and usually live longer, and thus have more time to develop late effects. There remain several important unanswered questions about cancer treatment in TYAs, some of which are detailed in box 1.
Box 1: Unanswered questions about cancer treatment in teenagers and young adults (TYAs)
What is the optimal fertility preservation strategy for girls and young women?
Should TYAs with cancer be treated with the same chemotherapy schedules as children or adults with cancer?
How will the expanding use of targeted drugs change late effects seen after chemotherapy in TYAs?
What are the late effects of chemotherapy?
Cardiovascular disease
Chemotherapy is associated with delayed cardiovascular complications including coronary artery disease, ventricular failure, and hypertension.8 A Danish cohort study of more than 43 000 TYA cancer survivors found an absolute excess risk of up to 400 extra hospitalisations due to cardiovascular disease per 100 000 person-years in survivors compared with the control group.9 A similar US study identified a twofold increased risk of cardiovascular disease, which adversely affected survival.10 These associations have been confirmed in specific cancer subtypes such as Hodgkin’s lymphoma and testicular cancer,11 12 where treatment regimens often contain anthracyclines and cisplatin.
The estimated risk of cardiac complications in TYAs is compounded by the fact that some patients will also receive mediastinal radiotherapy. In a study of Hodgkin’s lymphoma survivors, the actuarial risk of congestive heart failure 25 years after diagnosis was 0.4% with non-anthracycline chemotherapy without mediastinal radiotherapy, 7.5% with non-anthracycline chemotherapy and concurrent mediastinal radiotherapy, and 10.7% with anthracyclines and mediastinal radiotherapy.11
Identifying and managing cardiovascular complications
Regardless of therapy received, offer all TYA cancer survivors lifestyle advice to reduce their risk of cardiovascular disease. These recommendations are summarised in the infographic along with potential symptoms and monitoring advice, and are based on consensus guidelines. Robust evidence showing the effectiveness of prevention strategies does not yet exist. Consider coronary artery disease in all patients who present with chest pain regardless of age if they have a history of chemotherapy. There are no standardised guidelines for ventricular function screening after chemotherapy, but offer this to high risk patients, such as those with a history of anthracyclines or mediastinal radiotherapy. Systolic function can be assessed by echocardiography or a MUGA (multigated acquisition) scan (infographic).4 Offer women with any of the risk factors above who become pregnant echocardiography in the second trimester. For the management of left ventricular dysfunction, the best evidence supports ACE inhibitors with β blockers.13 14 A recent, single centre, prospective study of 2625 patients showed that early detection and therapy for anthracycline induced cardiac failure led to substantial recovery of cardiac function.15
Fertility
Loss of fertility can be distressing to cancer survivors.16 17 Chemotherapy induced infertility occurs primarily due to dose dependent gonadal toxicity, and alkylating agents such as cyclophosphamide and procarbazine are often implicated.18 For example, the MOPP (Mustargen, Oncovin, procarbazine, prednisone) regimen for treating Hodgkin's lymphoma included alkylating agents and led to 20% amenorrhoea rates in women.19
The Childhood Cancer Survivor Study found the relative risk of long term survivors becoming pregnant was 0.81 compared with healthy sibling controls. TYAs comprised 20% of the study cohort.20
The risk to fertility after chemotherapy generally increases with age at treatment.21 22 In a study of women with Hodgkin's lymphoma, the cumulative risk of premature menopause five years after treatment was higher among those aged 22-28 years than in those aged 14-21 years (27.2% v 5.6%).21 Other factors such as concurrent radiotherapy to the gonadal region 23 also affect risk. Online risk calculators (see www.fertilehope.org/tool-bar/risk-calculator.cfm) are available to estimate an individual patient’s risk. These calculators take into account gender, cancer type, and treatment and can be used by patients and health professionals.
Discuss fertility preservation early when agreeing a management plan and, given that treatment plans may change and that few regimens carry no risk of infertility, offer urgent referral to fertility preservation services for all TYA patients receiving any chemotherapy.24 25 Options for fertility preservation are outlined in table 2⇓.
Comparison of fertility preservation strategies in women
Second malignant neoplasms
Some 17-19% of all new primary cancers occur in cancer survivors.35 The reason why TYAs are at a greater risk of developing second malignant neoplasms than older survivors is unclear but may be because they receive more intensive drug schedules or because a proportion of patients already have a genetic predisposition to cancer. Data from the Surveillance, Epidemiology, and End Results (SEER) database, which includes details of more than two million cancer survivors, show that the relative risk of second malignant neoplasm decreases with increasing age at primary cancer diagnosis. For instance, for the three age groups 0-17, 18-29, and 50-59 years, the relative risk of second cancer decreased from 6.13 to 2.92 to 1.27 respectively.35 The absolute risk varies by type of both primary and second malignant neoplasm—primarily a consequence of the increasing incidence of most cancers with increasing age.36
Quantifying the risk of second malignant neoplasm from specific chemotherapy regimens is difficult because TYA cancer survivors may be at risk of second cancers due to genetic or environmental factors.37 Moreover, many protocols include radiotherapy, which itself is carcinogenic.38 However, several drugs have well established associations with a range of solid tumours.37 Alkylating agents, topoisomerase II inhibitors, and antimetabolites have been shown to induce therapy related acute myeloid leukaemia and myelodysplastic syndrome.39
Currently the only guidelines that exist for screening of second malignant neoplasms are for women at risk of breast cancer having received thoracic radiotherapy. This primarily includes female survivors of Hodgkin’s lymphoma and involves yearly mammogram and magnetic resonance imaging (MRI) from eight years after treatment or from age 25 years, whichever occurs later.4 In other patients, offer advice and support on lifestyle modifications known to reduce cancer risk including smoking cessation, alcohol use, sun exposure, diet, and exercise. TYAs are recommended to follow cancer screening guidelines applicable to the general population. More intensive screening may be needed for patients with genetic predisposition to cancers.
Neurocognitive effects
Neurocognitive changes after chemotherapy can affect survivorship.40 Antimetabolites and anthracyclines have been implicated. Although the association has long been established in childhood cancers,41 emerging evidence shows a similar effect in TYAs. A retrospective study of more than 2500 cancer patients aged 11-21 identified deficiencies in emotional regulation, memory and task efficiency.40 These individuals are likely to require additional psychological and social support (see infographic).
Fatigue
Cancer related fatigue is defined as a “distressing, persistent, subjective sense of physical, emotional, and/or cognitive tiredness or exhaustion related to cancer or cancer treatment that is not proportional to recent activity and interferes with usual functioning.”42 A recent systematic review highlighted that fatigue can be a disabling problem in younger patients with cancer, and that urgent research is needed to identify effective management strategies.43 Fatigue affects 17-29% of all cancer survivors,44 and can have a great effect on quality of life and function.44 Reversible causes should be explored (see infographic). Short bursts of exertion may be more manageable in these patients, and structured exercise routines, such as a moderate walking exercise programme, have proved to be helpful in improving fatigue and decreasing anxiety.44
Psychosocial effects
It is difficult to untangle which psychosocial effects are a direct side effect of therapy as opposed to the physical and psychological sequelae of cancer diagnosis and treatment during a period of life associated with much change. A recent systematic review on this subject subdivides adolescents and young adults into three groups based on social needs.45 The review found that mid-adolescents (15-17 years old) are principally coping with the physical changes of puberty and the formation of a social identity,46 whereas emerging adults (18-25 years old) are often in the process of leaving their childhood home, obtaining higher education, and establishing social connections independent from childhood.
Social effects
A multicentre observational cohort study of TYA cancer survivors in the US found that, although over 72% of patients previously in full time employment or education had been able to return to full time enrolment at 15-35 months after diagnosis, more than half of this cohort reported difficulties with work or education, including problems with forgetting, keeping up, and paying attention.47 In the same study, over 60% of 498 survey respondents experienced a negative impact of cancer on their financial situation.48 Financial issues may become apparent through disruption at work and/or difficulties in obtaining life insurance policies and mortgages.
Maintaining or forming close or sexual relationships with peers and potential life partners can be an issue. A negative body image due to cancer was reported by 61% of patients in the AYA HOPE study.48 This may be associated with specific treatment side effects such as alopecia.46 Any cognitive problems related to treatment may also hinder acquisition of social skills and lead to further problems with self esteem.49
Psychological effects
Psychological issues among TYA cancer survivors include stress, anxiety, and depression, which may relate to the disruption of life goals, interpersonal relationships and self image, as well as fear of disease recurrence.49 In a recent Australian cross sectional study, 48% of cancer survivors aged 15-25 years fulfilled the diagnostic criteria for post-traumatic stress disorder (PTSD),50 and the risk factors included female sex, less social support, and issues with self image and identity. The parents of these cancer survivors also had a 42% rate of PTSD, highlighting the need for family based psychological assessments and interventions.
A Canadian registry based study found that TYA cancer survivors were more likely to take antidepressants than healthy controls.51 Social isolation is also observed among TYA cancer survivors, who may wish to connect with other TYAs with similar experiences.52 However, this may cause negative psychological effects if peers relapse or die.
How can we best manage the psychosocial effects?
The US National Comprehensive Cancer Network guidelines recommend that TYAs should be involved in decision making from an early age, given age-appropriate information, and specifically asked about their understanding of the information and for permission to share it with parents and others.53 Patient empowerment is important in optimising survivorship. TYAs may also wish to access self help groups or online peer support to connect with cancer patients or survivors of a similar age, as well as benefit from advice on how to discuss their diagnosis with others.52
US data suggest there is inadequate provision of psychological support to serve the needs of TYA cancer patients,54 although corresponding UK data are lacking. The UK National Institute for Health and Care Excellence (NICE) recommends psychosocial needs assessment for patients up to the age of 24 years, and for their families or carers, and to offer appropriate specialist support at “key points” of care including long term follow-up,55 as well as early referral to fertility services.
Offer practical support, including referral to occupational health and social services (see infographic), and highlight sources of reliable information. Available resources range from tools for emotional self help, lists of counsellors, and support material for carers and family members, to information on fertility preservation, reasonable adjustments at work, insurance and mortgage issues, and benefits and financial assistance (such as free prescriptions for patients requiring treatment for side effects from cancer therapy).
How can we personalise long term care?
Given that TYA cancer patients may develop a wide array of complex late effects, there is an increasing move among care providers, worldwide, to formulate individualised long term care plans for patients. These care plans would be developed between patients and their multidisciplinary care teams at the end of treatment. These plans can be shared with the patient and primary care provider and would include detail about the treatment regimen, potential late effects, and an individualised plan for monitoring. In the UK this forms part of the recovery package devised by the National Cancer Survivorship Initiative, which includes a standardised holistic needs assessment of each patient after their treatment (including medical, psychological, and financial assessments) and an initial cancer care review carried out at the patient’s general practice three to six months after cancer diagnosis.56 Similar survivorship initiatives have been launched in other countries, all with the overarching aim of supporting TYA cancer survivors to live a healthy and productive life (supplementary table B).
A patient's perspective
I was diagnosed at 14 years old with stage four Hodgkin's lymphoma and received six rounds of chemotherapy and two weeks of radiotherapy. After six months in remission, I relapsed and was treated with alternating IEP and ABVD chemotherapy, followed by high dose BEAM chemotherapy and a stem cell transplant.
During the course of my treatment, I missed almost two full years of education and was unable to take my GCSEs. I have found it far more difficult to be around people, developing social anxiety and depression, for which I am being treated with medication and cognitive behavioural therapy. Having self confidence and dealing with my frustration is difficult, and I feel that I am a burden to my friends and family. It may help to have services within oncology that help with the emotional side effects while within the service, rather than after it.
I’ve also struggled with fatigue and have found it hard to work, even part time, and concentrate on my A-levels. Within the service, there is not enough focus around fertility, and I have struggled to cope with being infertile, especially since no measures were taken to help prevent it due to my age. Having osteoporosis has been difficult too. However, the Teenage Cancer Trust has really helped me with my recovery and finding out how to be a person and not a patient, again.
Lily Anderson—TYA cancer survivor
Additional educational resources for patients
Age-specific
Teenage Cancer Trust, UK charity (www.teenagecancertrust.org/)—Resources for cancer patients aged 13-24 years, including information on cancer types and treatments; patient stories by tumour type; advice on talking to peers, family, and doctors; information for friends and family; links to support programmes and events
CLIC Sargent, UK charity (www.clicsargent.org.uk/content/young-people)—Resources for cancer patients aged 16-24 years, including patient stories; Facebook group; online community; information about one-to-one social, emotional, practical, and financial support; free holidays
Further useful links to sources for support for issues including: emotional support, fertility, body image, relationships, finances
Teens Unite Fighting Cancer, UK charity (http://teensunitefightingcancer.org/)—Resource for cancer patients aged 13-24 years, including patient stories; blog; forum; support with provision of real hair wigs; national events
JTV Cancer Support, UK project with increasing links to other countries (http://jtvcancersupport.com/)—Online film-based resource for TYA cancer patients providing an extensive collection of videos by patients, their families, and healthcare professionals by cancer type, geographical region, topic, or “channel”
General
Cancer Research UK (www.cancerresearchuk.org/)
Macmillan Cancer Support, UK charity (www.macmillan.org.uk/)
Comprehensive resources including physical and psychosocial coping and support during and after treatment, including financial support; benefits; grants; mortgages; insurance; travel; fertility preservation; physical and sexual health; emotional help; helpline; online community
Additional educational resources for healthcare professionals
National Institute for Health and Care Excellence. Improving outcomes in children and young people with cancer (NICE guideline CSG7). 2005. www.nice.org.uk/guidance/csg7
Coccia PF, Altman J, Bhatia S, et al. Adolescent and young adult oncology. Clinical practice guidelines in oncology. J Natl Compr Canc Netw 2012;10:1112-50
Teenage Cancer Trust. Professional resources. 2012. www.teenagecancertrust.org/about-us/what-we-do/professional-leadership/professional-resources
National Institute for Health and Care Excellence. Cancer services for children and young people (NICE quality standard QS55). 2014. www.nice.org.uk/guidance/qs55/
National Cancer Intelligence Network. Cancer in children, teenagers and young adults (links to publications). 2010. www.ncin.org.uk/cancer_type_and_topic_specific_work/cancer_type_specific_work/cancer_in_children_teenagers_and_young_adults/
How patients were involved in the creation of this article
A Facebook group used by teenage and young adult (TYA) cancer survivors in our region was used to ask if any TYAs would be interested in sharing their views and helping to write the manuscript. One responder has written a patient story while another provided detailed advice on how to focus the article (in particular to focus on psychosocial aspects of survivorship) and reviewed and made suggestions to the final version. These comments specifically ensured that the article highlighted that the list of late effects in the infographic did not include every side effect possible and that the psychological effect of having peers who die during or after treatment is important.
Education into practice
Do you offer cardiovascular and cancer prevention advice to teenage and young adult (TYA) cancer survivors to help reduce their risk of late effects such as cardiovascular disease and second cancers?
Do you know how to refer to local fertility services for TYAs who will receive cytotoxic chemotherapy?
Ongoing research studies (a small selection of ongoing trials for teenagers and young adults from Australian, UK, and US trial programmes)
A study looking at how genes may affect the risk of kidney damage in children or young people who have treatment with ifosfamide (PK 2007 02)
A pilot randomized controlled trial of the Promoting Resilience in Stress Management (PRISM) intervention for adolescents and young adults with cancer—Study to investigate the effectiveness of the PRISM intervention, which is aimed at promoting self perceived resilience and consequently minimise patient distress
RITHM, resonance imaging trial for heart biomarkers in adolescent/young (AYA) cancer survivors—Study aimed at identifying asymptomatic patients with cardiovascular disease using MRI
Mobile health fitness program for adolescent and young adult childhood cancer survivors (TLC FIT)
Music therapy video development in improving communication, emotional distress, and recovery in adolescents/young adults undergoing treatment for high-risk cancer and their parents
Risk of fatigue in adolescent and young adult Hodgkin lymphoma patients
Care after lymphoma (CALy) trial—Phase II pilot randomised controlled trial of a lymphoma nurse-led model of survivorship care
Footnotes
We thank Jane Robson and Andre Jansen, TYA specialist nurses at Addenbrooke’s Hospital, for their help in writing the article; Charlotte Butterworth, a teenage cancer survivor who offered a great insight into how to write the article; and Lily Anderson, a teenage cancer survivor who wrote the patient story.
Contributors: SSA acts as guarantor. SSA planned the article, wrote the initial draft and performed literature review. MAVR helped write the initial draft and devised the tables. HMH planned the article and reviewed the initial draft. TVA planned the article and reviewed all drafts and approved the final article.
Funding: SSA is supported by the Cambridge Cancer Centre.
Competing interests: We have read and understood BMJ policy on declaration of interests and declare that we have no competing interests.
Patient consent obtained.
Provenance and peer review: Commissioned; externally peer reviewed.
This is an Open Access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 3.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/3.0/.
