Abstract
Sport is the leading cause of injury among adolescents and girls incur more non-contact anterior cruciate ligament (ACL) ruptures than boys, with this gender disparity in injury incidence apparent from the onset of puberty. Although the mechanisms for this gender disparity in ACL injuries are relatively unknown, hormonal, anatomical and biomechanical factors have been implicated. Puberty is associated with rapid skeletal growth and hormonal influx, both of which are thought to contribute to alterations in ACL metabolic and mechanical properties, as well as changes in lower limb strength and flexibility, ultimately influencing landing technique. Therefore, the aim of this review is to explain (i) the effects of changes in estrogen levels on the metabolic and mechanical properties of the ACL; (ii) changes in musculoskeletal structure and function that occur during puberty, including changes in knee laxity, and lower limb flexibility and strength; and (iii) how these hormonal and musculoskeletal changes impact upon the landing technique displayed by pubescent girls.
Despite evidence confirming estrogen receptors on the ACL, there are still conflicting results as to how estrogen affects the mechanical properties of the ACL, particularly during puberty. However, during this time of rapid growth and hormonal influx, unlike their male counterparts, girls do not display an accelerated muscle strength spurt and the development of their hamstring muscle strength appears to lag behind that of their quadriceps. Throughout puberty, girls also display an increase in knee valgus when landing, which is not evident in boys. Therefore, it is plausible that this lack of a defined strength spurt, particularly of the hamstring muscles, combined with the hormonal effects of estrogen in girls, may contribute to a more ‘risky’ lower limb alignment during landing, in turn, contributing to a greater risk of ACL injury. There is, however, a paucity of longitudinal studies specifically examining the lower limb musculoskeletal structural and functional changes experienced by girls throughout puberty, as well as how these changes are related to estrogen fluctuations characteristic of puberty and their effects on landing biomechanics. Therefore, further research is recommended to provide greater insight as to why pubescent girls are at an increased risk of non-contact ACL injuries during sport compared with boys. Such information will allow the development of evidence-based training programmes aimed at teaching girls to land more safely and with greater control of their lower limbs in an attempt to reduce the incidence of ACL ruptures during puberty.







Similar content being viewed by others
References
Emery CA, Meeuwisse WH, McAllister JR. Survey of sport participation and sport injury in Calgary and area high schools. Clin J Sport Med 2006; 16 (1): 20–6
Kelm J, Ahlhelm F, Anagnostakos K, et al. Gender-specific differences in school sports injuries. Sportverletzung Sportschaden 2004; 18 (4): 179–84
Michaud PA, Renaud A, Narring F. Sports activities related to injuries? A survey among 9–19 year olds in Switzerland. Inj Prev 2001; 7 (1): 41–5
Shea KG, Pfeiffer R, Wang JH, et al. Anterior cruciate ligament injury in pediatric and adolescent soccer players: an analysis of insurance data. J Pediatr Orthop 2004; 24 (6): 623–8
Powell JW, Barber-Foss KD. Sex-related injury patterns among selected high school sports. Am J Sports Med 2000; 28 (3): 385–91
Arendt EA, Agel J, Dick R. Anterior cruciate ligament injury patterns among collegiate men and women. J Athletic Train 1999; 34 (2): 86–92
Slauterbeck JR, Hickox JR, Beynnon B, et al. Anterior cruciate ligament biology and its relationship to injury forces. Orthop Clin North Am 2006; 37 (4): 585–91
Boden BP, Sheehan FT, Torg JS, et al. Noncontact anterior cruciate ligament injuries: mechanisms and risk factors. J Am Acad Orthop Sur 2010; 18 (9): 520–7
Chandrashekar N, Mansouri H, Slauterbeck JR, et al. Sex- based differences in the tensile properties of the human anterior cruciate ligament. J Biomech 2006; 39 (16): 2943–50
Deie M, Sakamaki Y, Sumen Y, et al. Anterior knee laxity in young women varies with their menstrual cycle. Int Orthop 2002; 26 (3): 154–6
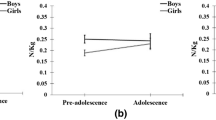
Ford KR, Shapiro R, Myer GD, et al. Longitudinal sex differences during landing in knee abduction in young athletes. Med Sci Sport Exerc 2010; 42 (10): 1923–31
Hewett TE, Myer GD, Ford KR. Decrease in neuromuscular control about the knee with maturation in female athletes. J Bone Joint Surg Am 2004; 86 (8): 1601–8
Hewett TE, Myer GD, Ford KR, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes. Am J Sports Med 2005; 33 (4): 492–501
Myer GD, Ford KR, Paterno MV, et al. The effects of generalized joint laxity on risk of anterior cruciate ligament injury in young female athletes. Am J Sports Med 2008; 36 (6): 1073–80
Quatman CE, Ford KR, Myer GD, et al. The effects of gender and pubertal status on generalized joint laxity in young athletes. J Sci Med Sport 2008; 11 (3): 257–63
Round JM, Jones DA, Honour JW, et al. Hormonal factors in the development of differences in strength between boys and girls during adolescence: a longitudinal study. Ann Hum Biol 1999; 26 (1): 49–62
Slauterbeck J, Clevenger C, Lundberg W, et al. Estrogen level alters the failure load of the rabbit anterior cruciate ligament. J Orthop Res 1999; 17 (3): 405–8
Malina R, Bouchard C, Bar-Or O. Growth, maturation and physical activity. 2nd ed. Champaign (IL): Human Kinetics, 2004
Dvorak J, George J, Junge A, et al. Age determination by magnetic resonance imaging of the wrist in adolescent male football players. Br J Sports Med 2007; 41 (1): 45–52
Hauspie R, Bielicki T, Koniarek J. Skeletal maturity at onset of the adolescent growth spurt and at peak velocity for growth in height: a threshold effect? Ann Hum Biol 1991; 18 (1): 23–9
Tanner J. Growth at adolescence. 2nd ed. Oxford: Blackwell Scientific Publications Ltd, 1962
Tanner JM, Whitehouse RH, Marubini E, et al. The adolescent growth spurt of boys and girls of the harpenden growth study. Ann Hum Biol 1976; 3 (2): 109–26
Taylor S, Whincup P, Hindmarsh P, et al. Performance of a new pubertal self-assessment questionnaire: a preliminary study. Paediatr Perinat Ep 2001; 15 (1): 88–94
Faust MS. Somatic development of adolescent girls. Monogr Soc Res Child 1977; 42: 1–90
Mirwald RL, Baxter-Jones ADG, Bailey DA, et al. An assessment of maturity from anthropometric measurements. Med Sci Sport Exerc 2002; 34 (4): 689–94
Gunther ALB, Karaolis-Danckert N, Kroke A, et al. Dietary protein intake throughout childhood is associated with the timing of puberty. J Nut 2010; 140 (3): 565–71
Iuliano-Burns S, Mirwald RL, Bailey DA. Timing and magnitude of peak height velocity and peak tissue velocities for early, average, and late maturing boys and girls. Am J Hum Biol 2001; 13 (1): 1–8
Kanbur NO, Derman O, Kinik E. The relationships between pubertal development, IGF-1 axis, and bone formation in healthy adolescents. J Bone Miner Metab 2005; 23 (1): 76–83
Jensen RK, Nassas G. Growth of segment principal moments of inertia between four and twenty years. Med Sci Sport Exerc 1988; 20 (6): 594–604
Hawkins D, Metheny J. Overuse injuries in youth sports: biomechanical considerations. Med Sci Sport Exerc 2001; 33 (10): 1701–7
Jensen RK. Growth of estimated segment masses between four and sixteen years. Hum Biol 1987; 59 (1): 173–89
Barber-Westin SD, Galloway M, Noyes FR, et al. Assessment of lower limb neuromuscular control in prepubescent athletes. Am J Sports Med 2005; 33 (12): 1853–60
McNair PJ, Marshall RN, Matheson JA. Important features associated with acute anterior cruciate ligament injury. New Zeal Med J 1990; 103 (901): 537–9
Liu SH, Al-Shaikh RA, Panossian V, et al. Estrogen affects the cellular metabolism of the anterior cruciate ligament: a potential explanation for female athletic injury. Am J Sports Med 1997; 25 (5): 704–9
Liu SH, Shaikh RA, Panossian V, et al. Primary immunolocalization of estrogen and progesterone target cells in the human anterior cruciate ligament. J Orthop Res 1996; 14: 526–33
Nigg B, Herzog W. Biomechanics of the musculo-skeletal system. Chichester: John Wiley & Sons, 1994
Smith BA, Livesay GA, Woo SL. Biology and biomechanics of the anterior cruciate ligament. Clin Sports Med 1993; 12 (4): 637–70
Liu SH, Yang R-S, Al-Shaikh R, et al. Collagen in tendon, ligament, and bone healing: a current review. Clin Orthop Rel Res 1995; 318: 265–78
Hamlet WP, Liu SH, Panossian V, et al. Primary immunolocalization of androgen target cells in the human anterior cruciate ligament. J Orthop Res 1997; 15 (5): 657–63
Faryniarz DA, Bhargava M, Lajam C, et al. Quantitation of estrogen receptors and relaxin binding in human anterior cruciate ligament fibroblasts. In Vitro Cell Dev Biol 2006; 42 (7): 176–81
Yu WD, Liu SH, Hatch JD, et al. Effect of estrogen on cellular metabolism of the human anterior cruciate ligament. Clin Orthop Rel Res 1999; 366: 229–38
Yoshida A, Morihara T, Kajikawa Y, et al. In vivo effects of ovarian steroid hormones on the expressions of estrogen receptors and the composition of extracellular matrix in the anterior cruciate ligament in rats. Connect Tissue Res 2009; 50 (2): 121–31
Seneviratne A, Attia E, Williams RJ, et al. The effect of estrogen on ovine anterior cruciate ligament fibroblasts. Am J Sports Med 2004; 32 (7): 1613–8
Toyoda T, Matsumoto H, Fujikawa K, et al. Tensile load and the metabolism of anterior cruciate ligament cells. Clin Orthop Rel Res 1998; 353: 247–55
Lee C-Y, Liu X, Smith CL, et al. The combined regulation of estrogen and cyclic tension on fibroblast biosynthesis derived from anterior cruciate ligament. Matrix Biol 2004; 23 (5): 323–9
Lee C-Y, Smith CL, Zhang X, et al. Tensile forces attenuate estrogen-stimulated collagen synthesis in the ACL. Biochem Biophys Res Commun 2004; 317 (4): 1221–5
Romani W, Langenberg P, Belkoff S. Sex, collagen expression, and anterior cruciate ligament strength in rats. J Athl Train 2010; 45 (1): 22–8
Woodhouse E, Schmale GA, Simonian P, et al. Reproductive hormone effects on strength of the rat anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc 2007; 15 (4): 453–60
Shelburne KB, Pandy MG, Anderson FC, et al. Pattern of anterior cruciate ligament force in normal walking. J Biomech 2004; 37 (6): 797–805
McNair PJ, Prapavessis H. Normative data of vertical ground reaction forces during landing from a jump. J Sci Med Sport 1999; 2 (1): 86–8
Beynnon BD, Bernstein IM, Belisle A, et al. The effect of estradiol and progesterone on knee and ankle joint laxity. Am J Sports Med 2005; 33 (9): 1298–304
Pollard CD, Braun B, Hamill J. Influence of gender, estrogen and exercise on anterior knee laxity. Clin Biomech 2006; 21 (10): 1060–6
Alter MJ. Science of flexibility. 2nd ed. Champaign (IL): Human Kinetics, 1996
Oatis C. Kinesiology: the mechanics and pathomechanics of human movement. 1st ed. Philadelphia (PA): Lippincott Williams & Wilkins, 2004
Uhorchak JM, Scoville CR, Williams GN, et al. Risk factors associated with noncontact injury of the anterior cruciate ligament. Am J Sports Med 2003; 31 (6): 831–42
Baxter M. Assessment of normal pediatric knee ligament laxity using the genucom. J Pediatr Orthop 1988; 8: 543–5
Falciglia F, Guzzanti V, Di Ciommo V, et al. Physiological knee laxity during pubertal growth. Bull NYU Hosp Jt Dis 2009; 67 (4): 325–9
Costello A, Grey A, Chiarello C. Anterior cruciate ligament laxity and strength of quadriceps, hamstrings, and hip abductors in young pre-pubescent female soccer players: a three-year prospective longitudinal pilot study. Orthop Prac 2011; 23 (1): 7–12
Ahmad CS, Clark AM, Heilmann N, et al. Effect of gender and maturity on quadriceps-to-hamstring strength ratio and anterior cruciate ligament laxity. Am J Sports Med 2006; 34 (3): 370–4
Loko J, Aule R, Sikkut T, et al. Motor performance status in 10 to 17-year-old Estonian girls. Scand J Med Sci Sport 2000; 10: 109–13
Heras Yague P, De La Fuente J. Changes in height and motor performance relative to peak height velocity: A mixed-longitudinal study of Spanish boys and girls. Am J Hum Biol 1998; 10: 647–60
Merni F, Balboni M, Bargellini S, et al. Differences in males and females in joint movement range during growth. Med Sport 1981; 15: 168–75
Volver A, Viru A, Viru M. Improvement of motor abilities in pubertal girls. J Sport Med Phys Fit 2000; 40 (1): 17–25
DeVita P, Skelly W. Effect of landing stiffness on joint kinetics and energetics in the lower extremity. Med Sci Sport Exerc 1992; 24: 108–15
Parker DF, Round JM, Sacco P, et al. A cross-sectional survey of upper and lower limb strength in boys and girls during childhood and adolescence. Ann Hum Biol 1990; 17 (3): 199–211
Seger JY, Thorstensson A. Muscle strength and electro- myogram in boys and girls followed through puberty. Eur J Appl Physiol 2000; 81 (1–2): 54–61
Ramos E, Frontera WR, Llopart A, et al. Muscle strength and hormonal levels in adolescents: gender related differences. Int J Sports Med 1998; 19 (8): 526–31
Barber-Westin S, Noyes F, Galloway M. Jump-land characteristics and muscle strength development in young athletes: a gender comparison of 1140 athletes 9 to 17 years of age. Am J Sports Med 2006; 34 (3): 375–84
Louw Q, Grimmer K, Vaughan C. Knee movement patterns of injured and uninjured adolescent basketball players when landing from a jump: a case-control study. BMC Musculoskelet Disord 2006; 7: 22–8
Pappas E, Sheikhzadeh A, Hagins M, et al. The effect of gender and fatigue on the biomechanics of bilateral landings from ajump: peak values. J Sport Sci Med 2007; 6: 77–84
Cowling EJ, Steele JR, McNair PJ. Effect of verbal instructions on muscle activity and risk of injury to the anterior cruciate ligament during landing. Br J Sports Med 2003; 37 (2): 126–30
Ford KR, Myer GD, Hewett TE. Valgus knee motion during landing in high school female and male basketball players. Med Sci Sports Exerc 2003; 35 (10): 1745–50
McLean SG, Huang X, Su A, et al. Sagittal plane biomechanics cannot injure the ACL during sidestep cutting. Clin Biomech 2004; 19 (8): 828–38
Hewett TE, Myer GD, Ford KR, et al. Preparticipation physical examination using a box drop vertical jump test in young athletes: the effects of puberty and sex. Clin J Sports Med 2006; 16 (4): 298–304
Quatman C, Ford K, Myer G, et al. Maturation leads to gender differences in landing force and vertical jump performance: a longitudinal study. Am J Sports Med 2006; 34 (5): 806–13
Ford KR, Myer GD, Hewett TE. Longitudinal effects of maturation on lower extremity joint stiffness in adolescent athletes. Am J Sports Med 2010; 38 (9): 1829–37
Wild CY, Steele JR, Munro BJ. How are muscle activation patterns during dynamic landing movements affected by growth and development? Implications for lower limb injuries [abstract]. In: ASICS Conference of Science and Medicine in Sport; 2008 October 16–18, Hamilton Island, Australia. J Sci Med Sport 2008; 11 Suppl. 6: 54
Kernozek TW, Torry MR, Iwasaki M. Gender differences in lower extremity landing mechanics caused by neuromuscular fatigue. Am J Sports Med 2008; 36 (3): 554–65
McNitt-Gray JL, Hester DM, Mathiyakom W, et al. Mechanical demand and multijoint control during landing depend on orientation of the body segments relative to the reaction force. J Biomech 2001; 34 (11): 1471–82
Cowling EJ, Steele JR. Is lower limb muscle synchrony during landing affected by gender? Implications for variations in ACL injury rates. J Electromyogr Kinesiol 2001; 11 (4): 263–8
Steele JR, Brown JM. Effects of chronic anterior cruciate ligament deficiency on muscle activation patterns during an abrupt deceleration task. Clin Biomech 1999; 14 (4): 247–57
Gauffin HK, Tropp H. Altered movement and muscular-activation patterns during the one-legged jump in patients with an old anterior cruciate ligament rupture. Am J Sports Med 1992; 20 (2): 182–92
Jones S, Lyons R, Sibert J, et al. Changes in sports injuries to children between 1983 and 1998: comparison of case series. J Pub Health Med 2001; 23 (4): 268–71
Price R, Hawkins R, Hulse M, et al. The football association medical research programme: an audit of injuries in academy youth football. Br J Sports Med 2004; 38: 466–71
Boden BP, Torg JS, Knowles SB, et al. Video analysis of anterior cruciate ligament injury: abnormalities in hip and ankle kinematics. Am J Sports Med 2009; 37 (2): 252–9
Hewett TE, Torg JS, Boden BP. Video analysis of trunk and knee motion during non-contact anterior cruciate ligament injury in female athletes: lateral trunk and knee abduction motion are combined components of the injury mechanism. Br J Sports Med 2009; 43 (6): 417–22
Acknowledgements
No sources of funding were used in preparing this review. The authors have no conflicts of interest that are directly relevant to the content of this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wild, C.Y., Steele, J.R. & Munro, B.J. Why Do Girls Sustain More Anterior Cruciate Ligament Injuries Than Boys?. Sports Med 42, 733–749 (2012). https://doi.org/10.1007/BF03262292
Published:
Issue Date:
DOI: https://doi.org/10.1007/BF03262292